IVF is a method of in vitro fertilization where sperm are added to an egg. ICSI is the process of transferring a specific single sperm “manually” into an egg. If even in these programs the pregnancy attempt is not successful, the couple is asked to find a sperm donor.
Conclusion
For some unknown reason, there is a cliché in society that infertility is the woman’s fault. However, statistics have now proven that throughout the world, infertility occurs in 15% of the total population in each country, and 5% of them are genetic mutations and idiopathic causes, which are almost impossible to correct.
The ratio of male and female factors in the causes of infertility is 40:60, so you should not “shift” the blame onto someone else, this reason is common and must be solved together. With adequate treatment and timely consultation with a fertility specialist, the chance of occurrence increases many times over.
Video: Male infertility. Urologist, andrologist, sexologist Alexey Kornienko
ICD-10
N46

General information
– a violation of male reproductive function, expressed in the inability to have offspring. Most often, male infertility is a consequence of qualitative and quantitative changes in sperm in the ejaculate due to previous inflammatory diseases genital organs, infectious and chronic diseases, exposure to chemical factors on the body. In 40-50% of cases it is the cause of infertile marriage. It can result in family breakdown and personal tragedy.
One tenth of all couples are unable to conceive without medical help. At the same time, the share of female infertility accounts for 40%, and the share of male infertility 45%; the remaining 15% accounts for cases of immunological incompatibility of spouses and rare forms of infertility.

Functioning of the male reproductive system
The male reproductive cell is the sperm, it contains genetic information about the father. Genetic information is concentrated in the head of the sperm, and with the help of the tail, the sperm is able to move to reach the egg. Spermatogenesis occurs in the testes; First, the sperm passes through convoluted tubules, which gradually turn into straight tubules and then into the epididymis. The total length of the tubules is about 500 meters; thanks to the slow movement along the convoluted tubules, the sperm matures and becomes capable of fertilizing the egg. In the epididymis, sperm undergo the last stage of growth, after which they enter the seminal vesicles through the vas deferens, where they accumulate and mix with the epithelial secretion, which contains nutrients for sperm. From seminal vesicles seminal fluid evacuated at the moment of ejaculation, mixing with the secretion prostate gland, the resulting liquid is called semen.
From the above, it becomes clear that the main causes of male infertility can be either obstruction of the canal, in which sperm cannot be expelled from the urethra due to obstacles, or violations of secretory function at any stage.
Secretory form of male infertility
In the secretory form of male infertility, the testicles do not produce required quantity spermatozoa, as a result of which fertilization of the egg is impossible. This form of infertility is also spoken of in cases where sperm motility is impaired or they have structural defects.
A common cause of secretory male infertility is testicular varicose veins (varicocele). The outflow of venous blood through dilated veins is difficult, so congestion develops, blood supply is disrupted and testicular function is inhibited. Mostly, varicocele affects the left testicle, but over time the process spreads to the second healthy testicle. As a result, the function of both testicles is significantly inhibited, sperm production decreases and a secretory form of male infertility develops.
Since spermogram data is labile, the examination is repeated if necessary in order to obtain an objective assessment of the possibility of fertilization.
Treatment of male infertility
Insemination with donor sperm is used for male infertility caused by aspermia, azoospermia, oligospermia III degree and other severe disorders of spermatogenesis. If the spouse has diseases for which the birth of children is not recommended, such as genetic diseases, the birth of children with severe congenital malformations, or the stillbirth of children with signs of severe hemolytic disease due to the incompatibility of the spouses with the Rh factor.
To improve sperm performance, the ejaculate is divided into fractions, separating mobile forms by filtration, using several different portions of cryopreserved sperm. To improve the sperm parameters of a man who has undergone treatment for male infertility, agrinin, caffeine and prostaglandins are added to it.
The effectiveness of the introduction of native sperm is several times higher than with insemination with cryopreserved sperm, but when using cryopreserved sperm, its antigenic properties are reduced, which is used in the treatment of female or male infertility in couples in which women have antisperm antibodies. In this case, sperm is injected either into cervical canal, or intrauterinely one day after the date of expected ovulation.
Hormone therapy for male infertility
Hormonal therapy for male infertility is indicated for various disorders of spermatogenesis, mainly in cases of impaired sperm motility, as stimulation after correction of underlying diseases, and less often as the main treatment.
Hormone replacement therapy for the treatment of male infertility is indicated for hypogonadism, idiopathic disorders of sperm motility (pathozoospermia) and hypoandrogenism. With the blocking method of treating male infertility, a man takes drugs that suppress spermatogenesis for several months; after discontinuation, the qualitative and quantitative characteristics of sperm improve. Although this antifertility method is rarely used to treat male infertility.
Stimulating hormone therapy for male infertility is based on the administration of small doses of hormones that have a beneficial effect on metabolic and other processes, but do not affect the hypothalamic-pituitary system. Treatment of male infertility with hormones is long-term, at least 9 months, with monitoring of the effectiveness of therapy at least once every 3 months. Dosages and choice of drug and dosage regimen depend on the type of pathology and are prescribed individually. If the sperm concentration is less than 5 million/ml of sperm, if the motile forms of sperm are less than 20%, hormone therapy for male infertility is futile.
Surgical treatment of male infertility
For male infertility caused by varicocele, the outflow of venous blood from the testicles is surgically improved. As a result, congestion disappears, metabolism is normalized and spermatogenesis is restored. The testicular veins are either ligated, sclerosed, or ligated. The prognosis of surgery for unilateral varicocele is favorable; if the process is bilateral, then sometimes additional drug therapy for male infertility is required.
In case of cryptorchidism, surgery to descend the testicles into the scrotum is performed in early age, however, it is necessary to exclude Kallman syndrome and other congenital pathologies. The earlier the orchiopexy operation is performed, the fewer irreversible changes in the spermatogenic epithelium and the less likely it is that mature age treatment for male infertility will be required. If testicular reduction was performed after reaching three years old, then the treatment does not give good results and many men subsequently have to undergo treatment for male infertility. Treatment of cryptorchidism with gonadotropic hormones is ineffective.
When surgically treating inguinal-scrotal hernias, it is important to minimize the risk of trauma to the spermatic cord; if the operation is successful, then usually further treatment for male infertility is not required, since reproductive function is completely restored. If there are congenital anomalies of the urethra, then plastic surgery to restore the canal with the formation of an external opening on the head is enough so that at the moment of ejaculation the sperm falls on the cervix. If there is an area of narrowing of the urethra, then surgery male infertility involves performing anastomoses using endoscopic surgery. Surgeries on the vas deferens are used for obstructive azoospermia, additionally eliminating the cause of obstruction (cyst, area of inflammatory obstruction, etc.).
A joint visit to a psychotherapist during treatment of female or male infertility will create favorable atmosphere for conception. Since many couples, after learning about the temporary impossibility of having children, experience a crisis based on reproaches, loss of tenderness during sexual intercourse and a feeling of inferiority. Conversations with psychotherapists and psychologists will help maintain normal relationships in the family and find a way out of the current situation, for example, adopting a child or using donor material for conception. It is important to understand that the opportunity to be a father is an opportunity to raise a child, and not at all to be his biological parent. And, if for some reason a man, even after undergoing a course of treatment for male infertility, cannot become a biological father, then this does not mean that he is inferior. A psychologist will help overcome this crisis without additional difficulties (depression, alcoholism, divorce), because often, having come to terms with the inability to conceive a child, and using alternative methods to create full-fledged family, a healthy and long-awaited child is born.
Where to start? Modern science has proven that it is necessary to start by eliminating the male factor of infertility: it is easier and less expensive.
A little physiology
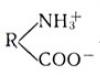
The sperm is a cell necessary for conception. It is produced by the male body. The sperm consists of a head, neck and tail. The head of the sperm contains all the genetic information that the father will pass on to his child. The tail of the sperm is needed for movement - so that it can reach the egg.
Sperm are produced in the convoluted tubules of the testicles, which are covered with germinal (sperm-forming) epithelium. Convoluted tubules become straight. The sperm must pass through these tubules in order to finally mature and become suitable for fertilization.
The total length of all tubules in each testicle is approximately 50 m. The straight tubules of the testis pass into the epididymis. In it, sperm finally mature and become able to enter the woman’s body and reach the egg. The vas deferens begins from the epididymis, passes through the inguinal canal, entering the abdominal cavity and flowing into the seminal vesicles, which are located behind the bladder. In the seminal vesicles, sperm accumulate and mix with the secretion of their walls. This secretion contains nutrients that sperm need on their way to the egg. From the seminal vesicles along the vas deferens, sperm pass through the prostate gland, also mixing with its secretions.
The resulting suspension of spermatozoa, chemical compounds And nutrients, which provide sperm with an alkaline environment, is called sperm. The vas deferens open into the urethra, into which sperm enters during ejaculation and is then forcefully expelled from the man’s body.
What is a spermogram?
First, a man takes a spermogram - the main test showing his fertility (i.e., ability to conceive). A spermogram can be taken at almost any medical institution that has urologists or andrologists on its staff. For greater accuracy of the spermogram result, it is necessary to carry out the analysis at least 2-3 times. Before each study, abstinence from sexual activity (including masturbation) should be at least 2, but no more than 5 days.
Let us dwell on the main indicators of the spermogram, as well as its possible deviations. Normal indicators spermograms:
- volume - 2-5 ml;
- pH - 7.2-8;
- VISCOSITY - UP TO 2 CM;
- liquefaction period - up to 60 minutes;
- sperm count - at least 20 ML/ML;
- total sperm count - at least 60 MILLION;
- sperm motility;
- rapid forward motion (A or 4) more than 25%;
- forward movement (A + B or 3.4) - more than 50%;
- morphology;
- normal sperm - more than 50%;
- agglutination - absent;
- leukocytes - no more than 1 million per ml;
- spermiogenesis cells - no more than 4% of the total;
- epithelial cells - single;
- red blood cells - absent.
The normal volume of ejaculate is 2-5 ml (about one teaspoon). A decrease in ejaculate volume may indicate decreased function of the testicles and gonads. With a semen volume of less than 2 ml, conception is extremely unlikely, even if other spermogram indicators are not changed.
The number of sperm in 1 ml of semen must be at least 20 million. A decrease in the number of sperm is called oligozoospermia. This is possible as a result of decreased testicular function or unilateral obstruction of the vas deferens. In the complete absence of testicular function or bilateral obstruction (i.e., obstruction of both vas deferens), azoospermia(complete absence of sperm in the ejaculate).
Doctors involved in the treatment of male infertility - urologists and andrologists - often have to answer the question of patients: if only one sperm is required for fertilization, why does reducing their number in sperm, say, to 1 million, make conception almost impossible?
During ejaculation, an average of 100 million sperm enter the cervix, and only half of them manage to overcome the mucous plug of the cervical canal. Of the remaining sperm, only small part reaches the fallopian tubes, and because The egg is located in only one fallopian tube, half of the sperm are again “wasted.” And again, not all sperm manage to get into the very fallopian tube. As a result, only about 200 sperm reach the egg. The likelihood of conception if there is only one sperm in the sperm is incredibly low. Having bought one lottery ticket, winning the main prize is much more difficult than buying a hundred.
Sperm motility is very important characteristic sperm quality. The norm is the movement of most of the sperm forward or, in extreme cases, chaotic movement. A decrease in the number of motile sperm is called asthenozoospermia, absence - necrozoospermia.
The number and motility of sperm in the ejaculate largely depends on the frequency of a man’s sexual intercourse. With frequent sexual intercourse, less mature forms of sperm enter the sperm, which have less mobility and viability.
The morphology (study of structure) of sperm shows what percentage of all sperm has a normal, complete structure. More than half of all sperm should also have a normal structure. A decrease in this indicator is called teratozoospermia.
You should not think that if sperm have structural defects, then the child may be born lame or with other disorders: the genetic material in them is completely complete. A decrease in the number of sperm with normal structure only reduces the likelihood of conception.
Agglutination, or gluing of spermatozoa with each other, is normally absent. The presence of agglutination sharply reduces sperm motility and the likelihood of conception. This is possible as a result of dysfunction of the gonads, which can develop against the background chronic prostatitis(inflammation of the prostate gland) and vesiculitis (inflammation of the seminal vesicles), as well as as a result of irregular sex life, specific inflammatory diseases, etc.
Sperm aggregation- areas of significant accumulation of sperm. Normally, aggregation should also be absent. The presence of areas of aggregation can sometimes be determined even by eye - these areas, compared to the bulk of the ejaculate, are distinguished by greater density and whiteness. Sperm aggregation often accompanies a decrease in their motility. It may also be a consequence various diseases and disorders in the male body.
White blood cell count, namely these cells are considered markers (indicators) of the inflammatory process, in the ejaculate should not exceed 1-2 in the field of view. Significant amount leukocytes may indicate acute inflammatory process urogenital tract. In this case, the doctor must conduct a thorough examination of the patient.
Most spermogram indicators are very labile, that is, they can change for many reasons, therefore, for an objective assessment of fertility, that is, the ability to fertilize, a man needs to repeat the study 2-3 times with a break of 14 days.
If abnormalities are detected in 2-3 spermograms, then it is necessary to establish their cause.
Only numbers
Disappointing statistics of the last decade show that every sixth marriage is infertile, that is, within a year of regular sexual activity without the use of contraception desired pregnancy doesn't come. In 50% of cases, the leading factor is the male factor, in 40% it is the female factor, and in 10% of cases both spouses have problems with reproduction.
Forms of infertility
There are several forms of male infertility:
- secretory;
- obstructive;
- immunological;
- mixed;
- idiopathic.
In the secretory form, the formation of sperm in the convoluted tubules of the testicles is impaired; in the obstructive form, there is an obstacle to their path to the urethra. At immunological infertility antibodies (i.e. killer cells) are produced to sperm in the woman’s body or in the man’s body itself. In the mixed form, fertility is affected by several factors at once, and the idiopathic form is cases of inability modern medicine install exact reason infertility.
Secretory form male infertility. In this form of the disease, the testicles do not produce the number of sperm needed to reach and fertilize the egg. Sperm motility may also be impaired, or most of them may have structural defects.
The secretory form of male infertility is always based on some effect on the testicles. The most common disease that interferes with sperm production is testicular varicose veins (varicocele). With this disease, excessively dilated testicular veins are not able to provide a complete outflow of blood from the testicle, as a result of which blood stagnation develops, the blood supply to the testicular tissue is disrupted and its function is inhibited. As a rule, varicocele is left-sided, but after some time the blood supply to the other testicle is disrupted. The result of this can be a significant decrease in sperm production by both testicles and, accordingly, a secretory form of infertility.
Similar phenomena are possible with hydrocele. With this disease, the scrotum accumulates a large number of fluid compressing the testicle. This compression can lead to disruption of the blood supply to the testicular tissue, which can ultimately result in male infertility. An inguinal hernia can give a similar result. A more rare disease leading to infertility is cryptorchidism - undescended testicles into the scrotum. Modern treatment cryptorchidism suggests that by the age of 7 it should be completely completed: the testicles must be in the scrotum. If this does not happen, testicular function may be significantly reduced.
Another disease that often leads to male infertility is mumps. The virus that causes this disease affects various glands of the body. Inflammation often occurs salivary glands, the patient's face takes on a rounded shape. The testicles in boys also become inflamed. If the inflammation of the testicles (orchitis) was severe enough, and the necessary treatment was not carried out, there is a danger of significant impairment of their function.
Damage to the germinal epithelium can also be caused by various external factors. Long-term exposure to radiation can cause not only radiation sickness and a wide variety of body disorders, but also severely damage the spermatogenic epithelium of the testicles, and this will lead to a significant decrease in the quality of sperm. Intense or long-lasting electromagnetic vibrations lead to the same thing. This is very important for those who like to carry mobile phones and other communication devices on their belts. Impact studies mobile phones on reproductive function men have not yet led to final conclusions, but it is possible that their result will not be encouraging.
High temperatures also negatively affect testicular function. It is worth paying attention to this not only for welders and stokers, but also for those who like to steam in a sauna or take a hot bath 2-3 times a week. Also, you should not overdo cycling training, especially if it is of a professional nature: this will also negatively affect the function of the genital organs. Compression and constant impacts of the perineum can lead to a decrease or complete disruption of testicular function, therefore, when treating this form of infertility, it is better to refrain from cycling and especially training. You should not wear tight underwear, because... it disrupts thermoregulation and presses the testicles to the body.
The following diseases lead to impaired spermatogenic function of the testicles:
- syphilis;
- tuberculosis;
- hormonal disorders;
- long-term use of antitumor, antiepileptic, some hormonal drugs and a number of antibiotics.
The reasons for a decrease in sperm count may be:
- prolonged stress;
- lack of protein and vitamins in food;
- unfavorable environmental factors;
- chronic lack of sleep;
- cigarette abuse, alcoholic drinks, drugs.
We must also not forget about genetically determined secretory infertility. This is Klinefelter syndrome (the presence of an extra X chromosome in a man); Del Castelo syndrome (isolated damage to the sperm-forming epithelium), etc.
Diagnosis of the secretory form of male infertility, in addition to a spermogram, often requires a testicular biopsy. This allows you to determine the condition of the testicular tissue and find out the root cause of the disease.
When treating the secretory form of male infertility, the cause of the disease must be eliminated - varicocele, testicular hydrocele; it is necessary to stop taking the negative effect medicinal product etc. After eliminating the cause, you need to carry out general course therapy to improve spermatogenic testicular function. The course includes not only good nutrition and normalization of lifestyle, but also vitamin therapy, as well as taking medications that improve blood supply to the scrotal organs. In some cases, stimulating hormonal and/or cell therapy is prescribed (for this, human hormone-producing cells cultured in the laboratory are used).
In general, treatment of the secretory form of male infertility is a very long, complex and painstaking, but by no means hopeless process.
Obstructive form of male infertility. With this form of infertility, the movement of sperm along the vas deferens on one or both sides becomes impossible. In case of unilateral obstruction of sperm patency, a decrease in the number of spermatozoa is observed; in case of bilateral obstruction, there is a complete absence of sperm.
The development of obliteration (obstruction of the vas deferens) occurs for a variety of reasons. Most often this happens as a result of epididymitis (inflammation of the epididymis). After the inflammation subsides, the ducts of the epididymis stick together or become blocked, as a result of which not a single sperm from the testicle can enter the seminal vesicles.
Also, injuries to the testicles or groin areas lead to this form of male infertility, especially if examination and/or treatment has not been performed. Often, obstruction of the vas deferens develops as a result of their accidental damage during surgery on the pelvic organs - bladder, ureters, rectum, etc. There are cases of compression of the vas deferens by a cyst or tumor of the epididymis. Not last place in the development of this form of male infertility is the congenital absence of the epididymis or vas deferens. Diseases that can cause such an unpleasant complication are syphilis and tuberculosis.
Diagnosis of obstruction of the vas deferens is carried out using special methods, with the help of which the presence, location and extent of the obliteration site are determined. Treatment of the obstructive form of male infertility is carried out by surgically restoring the patency of the vas deferens. The success of the operation depends on the length of the obliteration area. Depending on this, either an excision of a section of the vas deferens that is impassable for sperm is performed, or the formation of a new path for sperm is formed. For this purpose, they resort to anastomosis - the formation of an anastomosis with the opposite vas deferens.
Immunological incompatibility of partners. In 10% of cases of infertile marriages, none of the spouses has any diseases that could lead to infertility. Each of them may even have children from other marriages. The cause of infertility in such cases is most often the immunological incompatibility of partners (a woman’s allergy to sperm or other components of her husband’s sperm). To diagnose this form of infertility, analyzes and tests are used (MAP test, post-coital test, allergy test with the spouse’s ejaculate, etc.). Treatment of this form is successful in almost 100% of cases. The essence of the technique is to transfer the sperm directly into the uterine cavity (insemination).
Other forms.Male infertility may be due to some other reasons. For example, with hypospadias (the external opening of the urethra in a man is not at the top of the head of the penis, but below), sperm may not reach the cervix, as a result of which only a few sperm will be able to reach the uterus, which makes conception almost impossible. Hypospadia is treated surgically .
Male infertility can be caused by erectile dysfunction, in which it is impossible or difficult for a man to have sexual intercourse: an erection is absent or insufficient. Non-treatment of various inflammatory diseases, primarily urethritis and prostatitis, can lead to a similar result. With these diseases, men have no more than 1 full sexual intercourse per month. Accordingly, with such intensity of sexual activity, the likelihood of conception decreases.
It is also important that partners are sexually literate. There are people who are convinced that conception can occur not only with classic form sex, but also during anal and even oral sex. Frequent practice of these types of sex reduces the frequency of normal genital-genital contacts, as a result of which conception may not occur at all despite the best wishes of the spouses,
Idiopathic infertility. Idiopathic infertility is called infertility, the cause of which has not been established. Fortunately, the frequency of this form does not exceed 0.5-1%.
I would like to note that all couples without exception who want to have a child must undergo examination. In this area of human reproduction, self-diagnosis and self-medication are unacceptable. Modern science a whole range of alternative methods, which allow couples who are unable to conceive traditional way, achieve the desired result. As one example, we can mention the technique in vitro fertilization(IVF), in which only one sperm is needed for fertilization, which can even be taken directly from the testicle.
Studies of the effectiveness of treatment for all forms of infertility have shown that those couples who carefully followed all the recommendations and prescriptions of doctors had a desired pregnancy in 40-45% of cases.
A man’s inability to conceive a child is most often acquired in nature, arising as a result of diseases or under the influence of external factors. The most common cause is a violation of spermatogenesis - a secretory form of infertility in men, in which sperm are produced in insufficient quantities or have defects that make fertilization of the egg impossible.
At the second stage, the dilation of the veins is already noticeable in the absence of tension: tortuous weaves are visible under the skin of the scrotum. The size of the testicles does not change.
At the third stage, the testicle shrinks, its consistency changes, and the dilation of the veins is clearly expressed. The scrotum sags, pain is felt when walking, and potency deteriorates.
Starting from the second stage of varicocele development, a man feels bursting pain in the testicle, heaviness in the groin, and discomfort after sexual intercourse. Further, the symptoms intensify. Because of high blood pressure ruptures of blood vessels and hemorrhages into the scrotum occur in the veins. Lack of treatment leads to secretory infertility.
Starting from the second stage of varicocele development, a man feels bursting pain in the testicle and heaviness in the groin
Causes of varicocele
The appearance of varicocele can be caused by genetic factors, systemic diseases, mechanical damage, as well as organ pathologies.
External reasons that provoke dilation of the veins of the spermatic cord are:
- inguinal hernia;
- tumors;
- pressure on the veins of a crowded intestine with chronic constipation;
- prolonged abdominal muscle tension, chronic diarrhea;
- passion for horse riding and cycling;
- testicular injury;
- long periods of standing;
- compression of the renal vein.
Anatomical features can also have a negative impact:
- insufficiency of valves in the testicular vein or their complete absence;
- the testicular veins and the renal vein merge at right angles;
- The left testicular vein is significantly longer than the right one.
Some can cause varicocele venereal diseases(gonorrhea), autonomic disorders, weakness of vascular walls, decreased testosterone.
Diagnosis and treatment
Varicocele is diagnosed using ultrasound, venography, angiography. Research is being carried out to identify the primary causes (urography, hormone analysis). The degree of influence of the disease on spermatogenesis is determined by spermogram using fertility tests.
Conservative treatment aimed at improving blood flow is ineffective for severe varicocele. When there is a threat of infertility and severe pain, surgical methods are used, the purpose of which is to suppress dilated veins.
Varicocele is diagnosed using ultrasound
Hydrocele
The secretory form of infertility in men can be caused by testicular hydrocele (hydrocele). With this disease, serous fluid accumulates between the membranes surrounding the testicle. As a result, its size increases significantly. The shell is formed by two layers, one of which releases a certain amount of liquid, the other absorbs. The accumulation of contents above the norm creates excessive pressure in the testicle, as a result of which the process of spermatogenesis is disrupted.
Types of hydrocele
Dropsy can be congenital or developing due to anatomical abnormalities (primary), as well as occurring against the background of other diseases (secondary).
The congenital form of hydrocele is formed due to incomplete closure of the lumen of the processus vaginalis - part of the peritoneum, which is carried along with it into the inguinal canal by the testicle descending into the scrotum. Normally, this peculiar fold should heal, but in some cases the lumen remains open, which leads to the penetration of fluid into the membranes surrounding the testis. When partial overgrowth occurs, a cyst or hydrocele of the spermatic cord occurs, which also causes the development of secretory male infertility.
Acquired dropsy is of two types:
- idiopathic, in which excessive accumulation of fluid between the membranes of the testicle is caused by a violation of their absorption or excretory function due to age-related sclerotic changes, as well as obstruction of the lymphatic vessels;
- symptomatic, provoked by tumors, trauma, inflammation or heart failure.
Hydrocele of the testicle can appear after surgery to treat varicocele, as well as due to testicular torsion.
Hydrocele of the testicle can be congenital (primary) or occurring against the background of other diseases (secondary)
Symptoms and treatment
In the acute form of the disease, a rapid increase in testicular size occurs. The testis itself can no longer be palpated, and the skin of the scrotum becomes tense. Body temperature rises, pain is felt in the groin.
Hydrocele in chronic form is manifested by a slight increase in the size of the testicle, nagging pain in the area of the spermatic cord, discomfort when walking or sexual intercourse.
Hydrocele can develop into a hematocele or pyocele, which means an accumulation of blood or pus between the membranes of the testicle, respectively.
In some cases, dropsy (usually congenital) disappears on its own. If this does not happen, then the decision on surgical intervention is made by the doctor based on the results of the examination. The following methods are used:
- opening the membrane affected by dropsy and suturing its edges while preserving the functions of fluid exchange;
- excision of part of the membrane (during sclerosis).
A long course of the disease can cause not only secretory male infertility, but also complete testicular atrophy.
Inguinal hernia
An inguinal hernia (protrusion of part of the intestine into the inguinal canal) is often underestimated as a factor that can lead to male infertility. However, the protrusion gradually extends into the scrotum, enclosing the testicle and disrupting the blood supply and changing temperature conditions. Many people live even with a large hernia without experiencing much discomfort, only sometimes feeling a slight nagging pain.
But an inguinal hernia is dangerous not only because of strangulation, leading to necrosis of part of the intestine. Constant pressure on the vessels that supply sperm-producing testicular tissue gradually leads to the development of a secretory form of infertility.
The only reliable method of getting rid of an inguinal hernia is surgery. Moreover, in most cases, low-traumatic laparoscopy can be done.
Inguinal hernia is often underestimated as a factor that can lead to male infertility
Infectious diseases leading to secretory infertility
Disruption of the process of spermatogenesis can be caused by diseases such as syphilis, tuberculosis, sepsis, pneumonia, as well as infections transmitted through sexual contact. Developing in the body, pathogenic organisms provoke the production of antisperm bodies, damage the structure of sperm, and change the ejaculate.
Inflammatory processes in the above-mentioned diseases often result in the formation of scar tissue and adhesions, which causes obstruction (blockage) of blood vessels, ducts, and vas deferens. As a result, obstructive infertility in men develops simultaneously with secretory infertility.
Parotitis
The virus (paramyxovirus) mainly affects boys under 15 years of age, but in some cases adults also become ill. People call mumps “mumps.”
First of all, the virus spreading through the blood attacks the salivary and behind-the-ear glands, causing their inflammation. The next target is usually the testicles.
Against the background of the disease, the glands swell greatly, the face becomes puffy. The temperature may rise and aches in the joints may appear. But the insidiousness of the virus is that it can develop almost asymptomatically for 5-7 days, and obvious signs they do not always appear in the form of edema and increased salivation. Inflammation of the testicles (orchitis), which leads to secretory infertility, can arise as a complication already in active phase development of the disease.
Orchitis is an optional complication of mumps. Not every boy who has had mumps becomes infertile. The testicles become inflamed in 20% of cases, becoming painful and sometimes increasing in size by 3 times. This requires immediate medical intervention and hospital treatment. Advanced mumps can cause the death of testicular tissue and even their complete death. Timely, competent therapy with antiviral drugs will help avoid consequences such as infertility. Loss of fertility can be diagnosed only after puberty, but a doctor can give a fairly reliable prognosis in advance based on the degree of damage to the testis.
External factors influencing the development of secretory infertility
It happens that infertility develops in completely healthy man due to non-compliance with simple rules:
- Do not overheat the groin area and testicles. TO negative consequences Fertility can be affected by frequent visits to saunas and steam baths, long trips with heavily heated car seats, synthetic clothing, frequent hot baths;
- do not disrupt blood flow in the genitals. Pressure on blood vessels is caused by wearing tight underwear and trousers, horseback riding and long bicycle rides. A passive lifestyle also disrupts blood flow in the testicles: a man spends all his waking hours either sitting in an office chair or in a car;
- Do not wear radiating devices such as mobile phones on your belt. The spermatogenic epithelium of the testicles is damaged under the influence of electromagnetic vibrations;
- do not abuse alcohol and smoking. Bad habits disrupt spermatogenesis, imbalance hormonal background, lead to a deterioration in the patency and elasticity of blood vessels, including those supplying the testicles.
Secretory infertility can be the result of a lack of vitamins and protein, prolonged stress, unfavorable environmental conditions. But such factors are not fundamental, and in most cases aggravate existing diseases.
External provocateurs that inhibit testicular function also include medicinal and professional intoxications. In the first case negative impact sulfamilanides, cimetidine, long-term use of certain antibiotics and nitrofurans. Professional activity associated with the use of lead, mercury, manganese, benzene, ammonia, and phosphorus also impairs fertility.
If infertility is suspected, the first test that will decide the need for treatment is a spermogram. If the results of the study show low percentage viable sperm or their absence, then modern diagnostic methods will quickly identify the cause.
A good prevention of secretory infertility is an examination by a urologist and testing at least annually.
Do you have serious problems with potency?
Have you tried a lot of remedies and nothing has helped? These symptoms are familiar to you firsthand:
- sluggish erection;
- lack of desire;
- sexual dysfunction.
The only way is surgery? Wait, and do not act with radical methods. It is POSSIBLE to increase potency! Follow the link and find out how experts recommend treating...